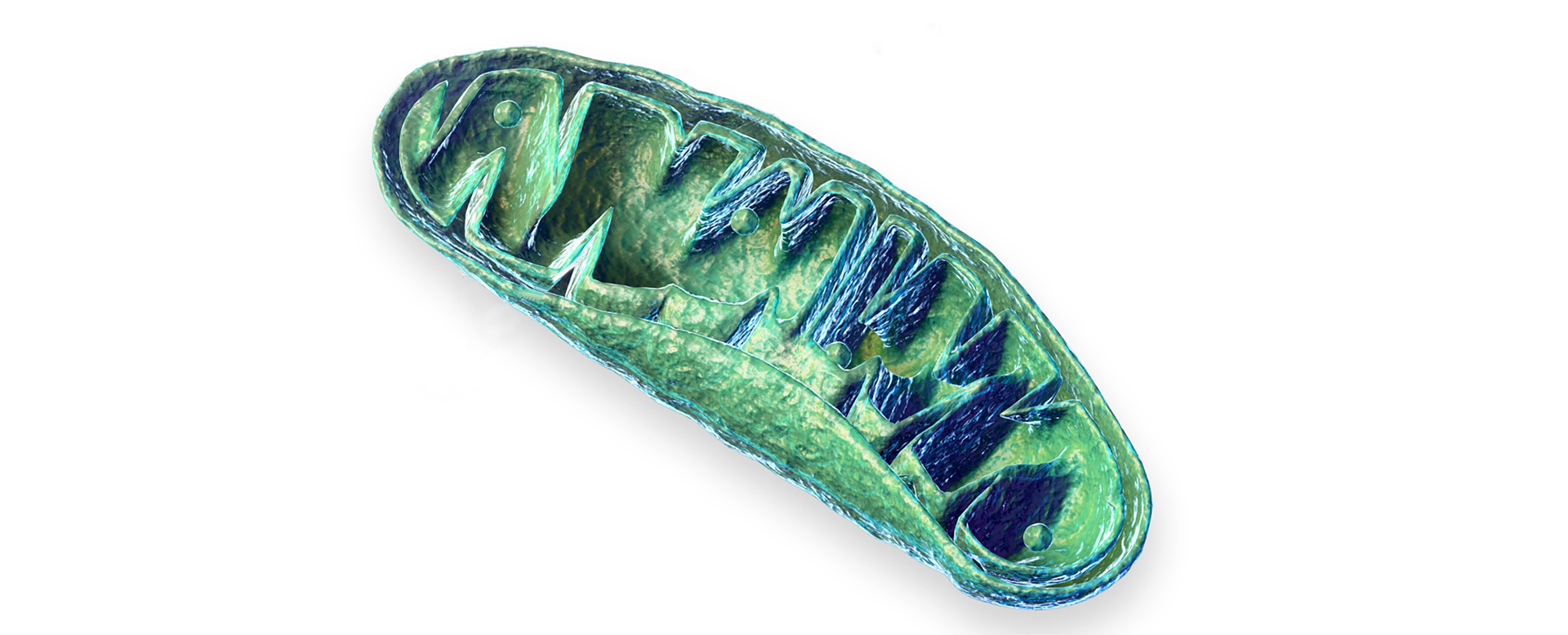
System’s science has fostered a paradigm shift; positioning mitochondria not only as powerhouses of the cell but also as organelles that influence, as well as reflect, the status of the entire body. Mitochondria are part of a structural and functional network1 comprised of the endoplasmic reticulum, the vacuole/lysosome and the peroxisome2, and the nucleus3. Moreover, they are “organelles in motion that function in specialized networks within the cell”,4 rapidly changing their location within a single cell, and between cells, by a number of different mechanisms.5
Mitochondrial signaling extends beyond bioenergetic pathways (eg. oxidation phosphorylation, the tricarboxylic acid (TCA) cycle and beta-oxidation of fatty acids) to numerous other pathways, including biosynthesis (eg. amino acids, nucleotides, cholesterol, glutathione), apoptosis, autophagy and mitophagy, antioxidant defense and cell signaling involving calcium ions and reactive oxygen species.6 They also act as molecular platforms integrating multiple innate immune signaling functions, including the control of inflammation.7 Indeed, mitochondria help regulate all innate immune signaling investigated so far in response to a broad spectrum of cellular insults including infection (bacteria and viruses) or sterile cell stress (mediated by the accumulation of damage-associated molecular patterns (DAMPs)).8 The interdependency between metabolic pathways taking place in mitochondria and the immune response is described in depth by a novel field of study termed immunometabolism.9
Identifying mitochondria as signaling organelles,10 regulating information flow not only within their associated cells but amongst adjacent cells, tissues and organs, indicate they also are part of a network within networks,11 capable of widespread influence throughout the entire body. Bidirectional communication pathways also exist between the mitochondria and microbiota12 as well as the extracellular matrix,13 further supporting a broad sphere of influence.
Being highly interconnected includes a number of trade-offs. For example, the ability of mitochondria to rapidly change their location, within, and between cells, increases their ability to produce energy exactly where, and when, it is needed. Being part of an interorganelle network bolsters the high degree of coordination needed to maintain functionality of critical cellular processes and adapt successfully when confronted with different stressors. Moreover, being part of a network of networks, suggests maintaining healthy mitochondria would have far reaching effects on the normal physiology, not only of local tissues but the whole body.
However, having a high degree of interconnectivity also means that widespread negative consequences could occur if mitochondria are dysfunctional. Mitochondrial dysfunction1 can be caused by different environmental toxicants (eg. certain fungicides, herbicides, pesticides, dioxins,14 and the common household antibacterial agent triclosan)15 as well as some pharmaceutical drugs (eg. HMG-coA reductase inhibitors as well as certain NSAIDs, analgesics, diabetes drugs, CNS drugs, antibiotics, antivirals, beta-blockers and cancer drugs).16
1 Secondary mitochondrial dysfunction is defined as caused by pathological events that originate outside the mitochondria or without an identified mtDNA or nDNA mutation in the genes encoding function or production of the OXPHOS proteins. This is in contrast to primary mitochondrial disease, defined as disorders impacting the structure or function of the mitochondria as a result of either nuclear DNA (nDNA) or mitochondrial DNA (mtDNA) mutations. Parikh S, Goldstein A et al. Diagnosis and management of mitochondrial disease: a consensus statement from the Mitochondrial Medicine Society. Genet Med. 2015;17(9):689-701
Mitochondrial dysfunction is associated with development of various diseases (eg. chronic fatigue syndrome, fibromyalgia, migraine, metabolic syndrome, neurodegenerative diseases such as Parkinsons disease and Alzheimer’s disease, autistic spectrum disorder, male infertility, bipolar disorder, inflammatory bowel disorders and cancer).6 In sum, mitochondrial integrity and function are critical to maintaining human health and homeostasis and mitochondrial dysfunction contributes to many disease states.4 A comprehensive treatment strategy to support mitochondrial function includes:
1) informing patients of known environmental toxicants, including certain pharmaceutical drugs, so that they can replace them or avoid them; 2) incorporating dietary and lifestyle choices that support mitochondrial health and 3) including various natural health products clinically verified to support mitochondria.
References
- Aon, M.A. Front Physiol. 2010;1(20):1-3
- Murley, A.A, and Nunnari J. Mol Cell. 2016;61(5):648-653.
- Saki M., and Prakash A. Free Radic Biol Med. 2017;107:216-227
- Trivedi M, Singh A et al. J Controlled Release. 2015;207:40-58
- Torralba, D., et al. Front Cell Dev Biol. 2016;4: eCollection 2016.
- Herst, P.M.et al. Front Endocrinol. 2017;8(896):1-16
- Jin, H.S, et al. Immune Network. 2017;17(2):77-88
- Monlun, M., and Hyernard C et al. J Mol Biol. 2017;429-1-13
- O’Neill L.A., et al. Nat Rev Immunol. 2016;16(9):553-565
- Chandel, N.S. BMC Biology. 2014;12:34
- Giao, J., et al. 2014;1:346-356
- Saint-Georges-Chaumet Y., and Edeas M. Pathog Dis. 2016;74(1):ftv096.
- de Cavanagh, E.M., et al. Am J Physiol Heart Circ Physiol. 2009;296(3):H550-H558
- Meyer, J.N., et al. Toxicol Sci. 2013;134(1):1-17
- Teplova, V.V., et al. Toxicol Lett. 2017;275:108-117
- Dykens, J.A. http://www.mitoaction.org/files/Dykens%20for%20Mitoaction.pdf (accessed Nov 2, 2017)