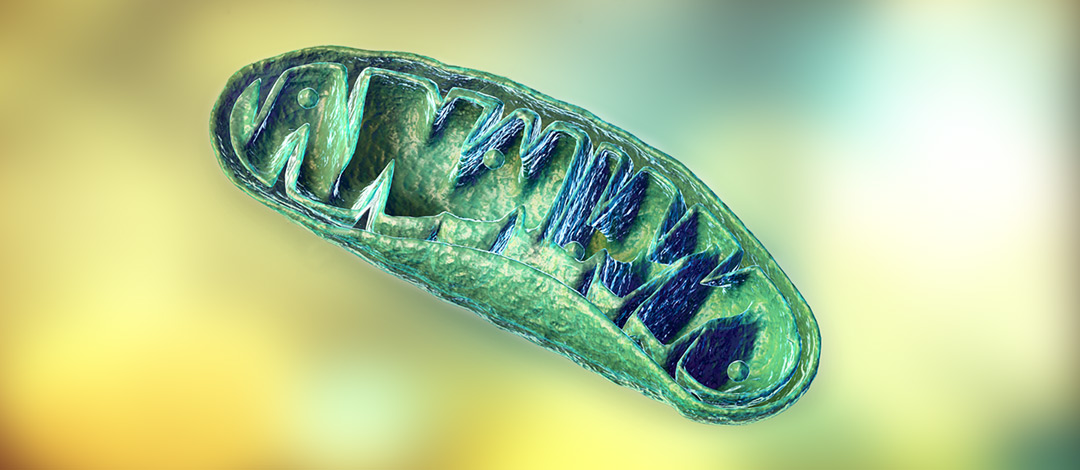
Historically, mitochondria were considered primarily as the ‘powerhouses of the cell’ because they contain the major biochemical pathways needed to produce ATP energy. However, mitochondria also have many other functions including biosynthesis of amino acids, nucleotides, cholesterol and glutathione as well as control of antioxidant defences, redox status, apoptosis and autophagy.1, 1 Mitochondria also are key controllers of the response to numerous stressors,2 including infection, tissue injury and metabolic dysfunction.3 This paper will summarize the recently discovered roles of mitochondria in regulating immune responses,4, 5 especially those necessary for fighting viral infections.
Mitochondrial signals that regulate immune responses include reactive oxygen species, proteins and peptides, lipids, ions, metabolites and even mitochondrial DNA when it is present in the cell cytoplasm or in the vascular system.5, 6 Mitochondrial dynamics, the change in mitochondrial shape, size and number,7 also regulate immune cell metabolism and functions5 and are essential to antiviral immunity.8 Mitochondria also signal by shifting locations within the cell or between cells via a number of different mechanisms9 as well as by regulating autophagy or mitophagy.1, 2, 5 Close bidirectional communication exists between mitochondria and the nucleus10 as well as between mitochondria and the microbiota.11
The early response to pathogens including viruses relies on mitochondrial signals. For example, different cells contain receptors on their surface or in their cytoplasm that recognize unique molecular patterns of various pathogens, including viral RNA of influenza A and coronaviruses. Activation of these receptors triggers intracellular pathways that use adapter proteins from the mitochondrial outer membrane named mitochondrial antiviral signalling proteins (MAVs). Stimulation of MAVs mediates synthesis and release of Type 1 interferons (IFN),12 key cytokines involved in clearing viral infections,13 as well as activates other important immune pathways including those associated with NF-kb and production of proinflammatory cytokines TNF-a, IL-1b, and IL-6.12 Other critical immune pathways including the assembly of inflammasomes3 such as NLRP3 also rely on signals integrated at the mitochondrial outer membrane. 5, 14, 15 For efficient antiviral defences, signals produced by or integrated by mitochondria play critical roles.8, 14
Various pathogens including medically important viruses such as influenza A and SARs-COV, attempt to escape antiviral defences via strategies that interfere with mitochondrial functions, including signalling via mitochondrial dynamics.8, 12 SARs-COV in particular affects mitochondrial dynamics as well as signalling by MAVs, contributing to suppression of the IFN response.16
The function of different types of immune cells including T cells, macrophages, dendritic cells and neutrophils is controlled by a balance between metabolic pathways such as oxidative phosphorylation in mitochondria and anaerobic glycolysis.5, 17 Cellular metabolism also has a central role in the function of natural killer (NK) cells, immune cells also critical in clearing viral infections.18 The discovery that cellular metabolism directly regulates the function and longevity of immune cells17 has led to development of a new scientific field named immunometabolism.19 Recent discoveries in immunometabolism support a close interdependent relationship between cellular metabolism and immunology for host defence,20 suggesting that altering metabolism through dietary means, nutritional supplements and physical activity would have a profound impact on the function of immune cells including those needed for defence against viral infections.
Mitochondrial health declines with age21 and mitochondrial dysfunction is a recognized contributor to suboptimal innate immune defences and chronic low levels of inflammation;22 this may be a contributing factor to an increased risk of severe infection in elderly populations. Current scientific research confirms that mitochondria are the powerhouses of immunity,5 in addition to being powerhouses of the cell. This evidence suggests that supporting mitochondrial health with dietary advice, specific nutritional supplements and other recommendations such as regular mild to moderate exercise may be an additional way to support optimal immune responses, especially during a period of increased risk of viral infections.
References:
- Herst PM, Rowe MR et al. Front Endocrinol. 2017;8(896):1-16
- Javadov S, Kuznetsov AV. Front Physiol. 2013:4(207):6-8
- Sandhir R, Halder A, Sunkaria A. Biochim Biophys Acta Mol Basis Dis. 2017;1863(5):1090–1097
- Weinberg SE, Sena LA, Chandel NS. Immunity. 2015; 42:406-417
- Mills EL, Kelly B, O’Neill LAJ. Mitochondria are the powerhouses of immunity. Nat Immunol. 2017;18(5):488–498
- Rodríguez-Nuevo A, Zorzano A. Cell Stress. 2019;3(6):195–207.
- Rambold AS, Pearce EL. Trends Immunol. 2017; pii: S1471-4906(17)30170-9
- Kim SJ, Ahn DG, Syed GH, Siddiqui A. Mitochondrion. 2018;41:21–27
- Torralba D, Baixauli F, Sanchez-Madrid F. Front Cell Dev Biol. 2016;4:107
- Quirós PM, Mottis A, Auwerx J. Nat Rev Mol Cell Biol. 2016;17(4):213–226
- Han B, Lin CJ, Hu G, Wang MC. FEBS J. 2019;286(4):630–641
- Lai JH, Luo SF, Ho LJ. Biochem Pharmacol. 2018;156:348–356.
- Kalliolias GD, Ivashkiv LB. Arthritis Res Ther. 2010;12 Suppl 1(Suppl 1):S1
- Monlun M, Hyernard C, Blanco P, Lartigue L, Faustin B. J Mol Biol. 2017;429(1):1–13.
- Holley CL, Schroder K. Clin Transl Immunology. 2020;9(2):e01109
- Shi CS, Qi HY, Boularan C, et al. J Immunol. 2014;193(6):3080–3089
- Loftus RM, Finlay DK. J Biol Chem. 2016;291(1):1–10
- O’Brien KL, Finlay DK. Nat Rev Immunol. 2019;19(5):282–290.
- O’Neill LA, Kishton RJ, Rathmell J. Nat Rev Immunol. 2016;16(9):553-565
- Mintern JD, Binger KJ. Clin Transl Immunology. 2020;9(3):e1123.
- Aon MA, Cortassa S et al. Clin Sci (Lond). 2016;130 (15):1285-1305
- West AP. Toxicol. 2017;391:54-63